CHPN Practice Exam
2025 Edition
Take this free CHPN practice test to get a sample of the types of questions on the actual Hospice and Palliative Nurse certification exam.
The CHPN exam is a 3 hour exam covering 150 multiple choice questions. The CHPN exam focuses on five domain practice areas: Life-limiting Conditions in Adult Patients, Pain Management, Symptom Management, Patient and Family Care and Practical Issues.
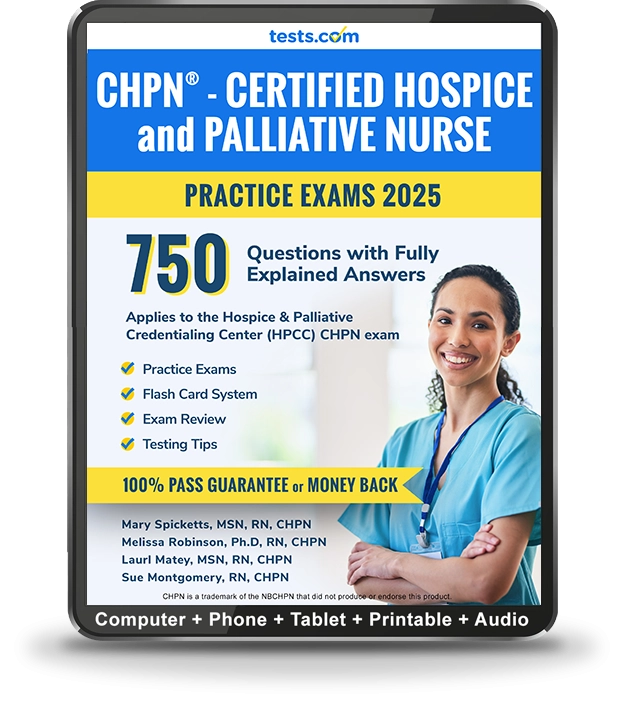
You can also try the Complete 750 Question CHPN Practice Exam Kit with fully explained answers, testing tips and more.